"My preschooler has an IEP and health issues. He has a chronic heart condition, so he can't run and jump around like other kids because he gets too tired. He has to take meds at lunchtime. The special educators and the teachers came up with some great strategies so he can participate and also rest." – Parent of a child with disabilities and special health care concerns
This chapter highlights the health and mental health services that are part of a coordinated approach for children with disabilities and their families. Your work as a disability services coordinator includes how the health and mental health regulations apply to children with disabilities.1 Your key partners are the health and mental health managers and the mental health consultant. In some programs, disability services coordinators also hold the position of health managers or mental health managers.
Key Ideas
- All health and mental health program services must be available to children with disabilities and their families.
- Collaboration with the health manager and the health team is essential to meet the needs of children with disabilities and their families.
- Responsive health and mental health services respect families' cultural beliefs and practices.
- Individualization is key to providing health or mental health services to all children, including those with disabilities.
- A mental health consultant has an important role working with staff and families.
- Early childhood mental health is synonymous with social and emotional development.
- Children with disabilities and their families may need help accessing appropriate health and mental health services.
- Breaking down stigmas associated with health or mental health issues is an important part of staff training and parent education.
- Quality health and mental health services are integral to a coordinated approach for children with disabilities and their families.
What are the health services in Head Start programs?
The HSPPS at 45 CFR §1302 Subpart D – Health Program Services require programs to provide high-quality health, oral health, mental health, and nutrition services to all children. All health services must be developmentally, culturally, and linguistically appropriate and support each child's growth and school readiness. Learning experiences and daily routines must include teeth brushing, nutritious meals and snacks, physical activity, and age-appropriate rest or quiet time.
Every program must have an Health Services Advisory Committee (HSAC) that includes Head Start parents, professionals, and community partners. The HSAC helps identify community health issues that affect Head Start families, find and access resources, and advise on program health policies and procedures.
Within 30 days of a child starting the program, staff must determine whether the child has access to continuous and accessible healthcare and health insurance. If not, the program must help the family access these supports.
Within 90 calendar days of a child's attending a center-based program or family child care home or receiving a home visit in a home-based program (or 30 days in a short-term program), a program must learn from professionals whether a child is up to date on:
- Primary medical and oral healthcare based on the well-child visits and dental periodicity schedules according to the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program of your state's Medicaid agencies
- Immunization recommendations from the U.S. Centers for Disease Control and Prevention (CDC)
- Additional recommendations from a program's HSAC based on community health problems
If children are not up to date on their well-child visits and dental periodicity schedules, a program is required to help parents arrange them or directly facilitate the child's health services.
A program must facilitate and monitor oral health preventative care, treatment, and follow-up, including topical fluoride treatments. Also, a program must identify a child's nutritional health needs.
Health services include screening and referral procedures as described in 45 CFR §1302 Subpart C – Education and Child Development Services. Within 45 days of a child's entry, a program must either obtain or administer vision and hearing screening. If health concerns are raised in a child's medical record or parent report, a program must facilitate further diagnostic testing, evaluation, treatment, and follow-up. A program must keep confidential records of referrals and services.
A program is required to collaborate with parents about their child's health and well-being. Parents must give consent for any procedures administered by a program. The HSPPS require a program to help parents:
- Learn about preventative care and children's health issues
- Promote their own well-being
- Navigate through health systems to meet their child's general health and identified needs
- Obtain adaptive equipment and varied services when needed
- Engage with family support programs
- Establish their eligibility for additional supports
The HSPPS at require staff and consultants who perform health procedures or support nutrition services to meet professional qualifications. A program is required to provide information to staff about mental health and wellness issues that may affect their job performance and to schedule regular opportunities to learn about health topics.
HSPPS Related to Health, Oral Health, and Nutrition
- Attendance, 45 CFR §1302.16
- Suspension and expulsion, 45 CFR §1302.17
- Child screenings and assessments, 45 CFR §1302.33
- Purpose, 45 CFR §1302.40
- Collaboration and communication with parents, 45 CFR §1302.41
- Child health status and care, 45 CFR §1302.42
- Oral health practices, 45 CFR §1302.43
- Child nutrition, 45 CFR §1302.44
- Staff qualifications and competency requirements, 45 CFR §1302.91
- Staff health and wellness, 45 CFR §1302.93
- Program procedures – applicable confidentiality provisions, 45 CFR §1303.21
- Disclosures with, and without, parental consent, 45 CFR §1303.22
 What are mental health services in Head Start programs?
What are mental health services in Head Start programs?
The primary HSPPS pertaining to mental health services appear in 45 CFR §1302 Subpart D – Health Program Services. They require programs to support a program-wide culture that promotes children's mental health, social, and emotional well-being. The regulations mandate that a program:
- Provide supports for effective classroom management and teaching strategies to support children with behaviors that are challenging or who manifest other mental health concerns
- Make available mental health consultation services to partner with staff and families
- Obtain parental consent for consultation services at the time of enrollment
- Build community partnerships to facilitate access to mental health resources and services
- Provide opportunities for parents and staff to discuss children's mental health issues, concerns about their child's behavior and development, and appropriate responses
The HSPPS describe the roles and responsibilities of the mental health consultants. They are required to:
- Assist the program to implement strategies to identify and support children with mental health concerns
- Use observation and consultation to address the concerns of teachers, family child care providers, and home visitors related to children's social and emotional development and effective strategies
- Help parents and staff understand mental health and access to interventions
- Assist in the implementation of policies to limit suspension and prohibit expulsion
 45 CFR §1302 Subpart I – Human Resources Management requires that a program use licensed or certified mental health professionals with knowledge and experience serving young children and their families. 45 CFR §1302 Subpart A – ERSEA regulations refer to suspension and expulsion policies and the mental health consultant's role to ensure children's full participation in the program. The HSPPS at 45 CFR §1302 – Subpart E Family and Community Engagement Services mandate that a program build relationships with child and adult mental health resources in the community.
45 CFR §1302 Subpart I – Human Resources Management requires that a program use licensed or certified mental health professionals with knowledge and experience serving young children and their families. 45 CFR §1302 Subpart A – ERSEA regulations refer to suspension and expulsion policies and the mental health consultant's role to ensure children's full participation in the program. The HSPPS at 45 CFR §1302 – Subpart E Family and Community Engagement Services mandate that a program build relationships with child and adult mental health resources in the community.
As part of the developmental screening process described in 45 CFR §1302 Subpart C, a program must assess social and emotional behavior during the first 45 days of enrollment. They may use a comprehensive screening tool or a specific screener for this purpose. Ongoing assessment data and information from the family also contribute to the child's social and emotional profile. Depending on the screening results and other information, a child might be referred for a follow-up evaluation to determine eligibility for IDEA services.
HSPPS Related to Mental Health Program Services
Planning for Partnerships
You are likely to collaborate with the health manager, mental health manager, and other staff to develop effective local partnerships.
- Get to know the members of the HSAC and their areas of expertise.
- Plan joint training to make consistent accommodations for children's health and mental health needs.
- Collaborate with mental health consultation services.
- Know what the process is for planning and communicating with children's medical, dental, and mental health providers and specialists.
- Communicate the key requirements of your programs' suspension and expulsion policies.
- Include parents' and family's voices in efforts to improve health and mental health services.
Partnering with the Health Team
As the disability services coordinator, your primary task is to ensure that all health services are made available to children with disabilities. Their oral health and nutritional needs must be addressed and immunizations up to date. Their families must have access to health services. You can help ensure that health concerns for all children, such as obesity and tooth decay, are addressed in appropriate ways with children with disabilities and their families. The health services are another piece of the coordinated approach.
Spread the word! The ECLKC provides tips about how to help children with disabilities brush their teeth and find comfortable positions. Share these resources with staff and families.
You don't do this work alone; you partner with the health manager, who is responsible for implementing quality health services grounded in the HSPPS. The exact nature of your collaboration varies from program to program, depending on its size and structure, job qualifications, and other factors. However, the health manager typically flags medical records that indicate health concerns and responds to parental concerns about their child's health. They review vision and hearing screening and identify children who need follow-up. The health manager is also the point of contact for children's medical and dental homes and with health resources in the community.
Refer to the Head Start Health Services Competencies for a description of the roles, responsibilities, and scope of work for health services staff.
Your partnership with the health manager helps you:
- Respond to the individual health needs of families of children with disabilities
- Develop partnerships with health professionals who work closely with children with disabilities or suspected delays
- Eliminate the barriers to health services for children with disabilities
- Promote a coordinated approach that ensures the full participation in program activities for children with disabilities and their families
You and the health team can encourage healthy eating, exercise, and rest. Look for ways to reduce staff stress at the program level. When caregivers take care of themselves, they are better able to care for young children. Plan health education opportunities with the health manager, other staff, and community resources. Provide learning opportunities to help break down barriers and stigmas associated with disabilities and medical or mental health conditions.
Children with Special Healthcare Needs
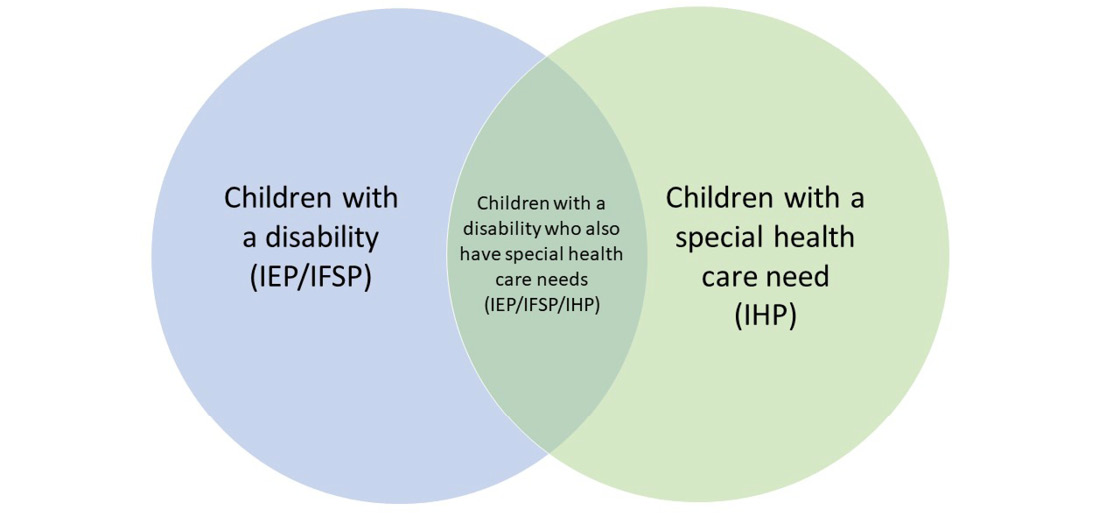
Children with special care needs may have Individualized Health Plans (IHPs). The health manager works with the child's primary medical provider to develop an IHP that describes medication protocols and health and safety practices. The IHP also specifies whether the child needs regular activity adaptations due to a medical condition. Some children with health concerns may be eligible for case management services under a Section 504 Plan,2 EPSDT, or other program. If children with health conditions have suspected delays that affect their learning, you can refer them to the local Part B or Part C agency for an evaluation. If they qualify for IDEA services, an IFSP or IEP would be prepared.
You and the health staff share the same goal—to individualize services for children and their families to ensure their inclusion in all program activities. Together, you can help teaching staff and home visitors accommodate learning experiences for children with disabilities and health concerns. You and the health manager are advocates for inclusive policies and practices across the program's services.
For example, if a child with feeding issues also has an IFSP or IEP, you can work with agency specialists and the health team to make sure the feeding issues are addressed clearly in an IHP. In this example, the child would be represented in the shaded area of the diagram above. Together, support teachers, family child care providers, and home visitors to include the children at snack and mealtimes. There may be children with disabilities whose health conditions limit their physical activity. Work with the early intervention, special education, and Head Start education staff to ensure their participation in learning opportunities on the playground.
What is your role in mental health services?
You ensure children with disabilities and their families receive mental health services that are available to all Head Start children and their families. The services are intended to promote positive, responsive relationships between a child, their peers, and adults in the program and between the child and family members.
Depending on the structure of your program, you may work directly with the mental health consultant, the health or mental health manager, and the education manager to respond to mental health concerns. In some programs, the disability services coordinator who meets the job qualifications also serves as the health or mental health manager.
You may manage or participate in the identification process for children referred for mental health concerns. Track where the children are in the process, just as you do for all referred children. See Appendix C for a sample tracking sheet. Work closely with your IDEA Part B special education partners or Part C early intervention partners to understand their eligibility criteria for social and emotional disorders, delays, and services. This helps your team decide who to refer for diagnostic evaluations. If you work with different school districts, the eligibility criteria may differ.
Depending on the circumstances, the child might be referred directly to a mental health clinic or other provider. Most likely, you will be part of a team that makes these referral decisions. The team might consist of the teachers, home visitors, mental health consultant, family service workers, and others who have contact with the child and the family. If children with mental health concerns don't quality for IDEA services, there are other options to explore. Some may qualify for a Section 504 Plan, or your program may develop an internal Child Action Plan.
Children's social and emotional issues are sometimes related to classroom organization and management. Working closely with the education manager and coaches helps ensure teaching staff or family child care providers implement a high-quality, supportive learning environment that builds positive adult-child relationships. In home visiting programs, help staff work with the family to provide a nurturing, responsive home environment. Communicate to staff and families that predictable schedules and familiar routines support all children's social and emotional development. For children with disabilities, a safe and secure environment affects their positive mental health.
Early childhood mental health is the same as social and emotional development.
Working with a Mental Health Consultant
Typically, program management prepares the contract for the mental health consultant and supervises their work. However, you may be asked to provide input based on your knowledge of the children with disabilities and their families in your program. In some programs, the disability services coordinator is also the mental health services manager, which is different from the mental health consultant.
An important part of your work is making sure staff and families know that they have access to a mental health consultant. This person does not work with the child but supports the caregiving adults. The consultant's role is to observe and consult. They can identify mental health concerns, provide support to staff and families, and help your program and families obtain services.
Early on, the consultant is likely to meet with your program director or leadership team to identify the most effective ways to meet your program's needs. As you work with staff and families, you are likely to get a sense of how to prioritize the consultant's services. Some centers or staff may need more support from the consultant. For example, if your program's ongoing assessment indicates frequent staff concerns in one center about children's behaviors that challenge adults, ask the consultant to spend more time observing in these classrooms and meeting with teachers. You and the management team also might ask the consultant to provide staff training.
Stay informed about Head Start's policies on temporary suspension and prohibition of expulsion due to a child's behavior. The HSPPS state that when a child's participation in the program is uncertain, a mental health consultant must be brought in. There may be times when you and the health or mental health team need to explain to staff and parents how your program implements these policies about suspension and expulsion.
For more information, refer to Suspension and Expulsion of Children with Disabilities or Suspected Delays. The relevant HSPPS and effective program strategies are clearly laid out.
Nurturing Social and Emotional Development
In some cases, a child has an identified social and emotional disability with an IFSP, IEP, Section 504 Plan, or internal Child Action Plan in place. However, in other cases, a different type of disability affects social and emotional development. For example, the child with a physical disability might be unable to keep up with peers on the playground. The child with a speech disability might not be able to communicate effectively with others. As a result, these children may feel rejected, frustrated, lonely, or anxious. Helping staff and families understand the complex relationship between disabilities and social and emotional development is part of your job.
Work with specialists, the mental health consultant, and other program staff to sort out these complexities. Remember that you are part of a coordinated effort. Together, you may identify effective strategies, such as:
- Making sure your program has accommodations in place that maximize positive interactions between children with disabilities and typically functioning peers
- Helping children with disabilities learn to regulate and verbalize their feelings
- Use the ELOF as a guide when creating social and emotional goals for children from birth to age 5
- Refer to the curriculum modifications discussed in Chapter VII
- Implementing a specific curriculum designed to promote social and emotional development
- Helping families and staff understand that some children with disabilities need additional support to cope with their emotions in the program and at home
- Individualizing services and learning opportunities for all children
Affirm that, first and foremost, children with mental health challenges are children. Hold up a strengths-based lens as you view a child. This helps reduce the stigma associated with mental health issues.
Behaviors That Challenge Us
 Education staff, as well as parents and family, may come to you with serious concerns about a child's behavior. They may be worried about a child who appears withdrawn and disengaged, often referred to as internalizing behavior. These behaviors are challenging to adults because they don't know what to do or how to help the child engage. Likely, this is a child who is not participating fully and effectively in all learning activities and may go unnoticed in a classroom. Working with the mental health consultant, you and educational staff can develop intentional strategies to engage the child, such as pairing with a peer during small-group activities.
Education staff, as well as parents and family, may come to you with serious concerns about a child's behavior. They may be worried about a child who appears withdrawn and disengaged, often referred to as internalizing behavior. These behaviors are challenging to adults because they don't know what to do or how to help the child engage. Likely, this is a child who is not participating fully and effectively in all learning activities and may go unnoticed in a classroom. Working with the mental health consultant, you and educational staff can develop intentional strategies to engage the child, such as pairing with a peer during small-group activities.
More frequently, teachers and parents are concerned about a child who displays externalizing behaviors. They report that a child is "negative, defiant, aggressive, destructive" and fear for the child's own safety, the safety of other children, or even that of staff. Teachers perceive these behaviors as challenging or disrupting in the group setting, and so they may exclude children who exhibit these behaviors from activities and isolate them from peers. Parents may resort to ineffective discipline techniques that sometimes escalate the child's behavior. Help staff and families understand that such responses from adults do not support inclusion.
The defining feature of children's challenging behavior is that adults perceive it as challenging. It is important for caregivers to remember that behavior has meaning. Some children's challenging behavior is typical for their age and stage of development, and adults can use appropriate guidance to address it. Other children's behaviors may indicate more serious concerns, and they may need further evaluation or treatment. (Adapted from the Mental Health Glossary.)
Reach out to the mental health consultant, special educators, and your program staff to support effective class management and strategies to redirect children's behavior. The HSPPS detail standards of conduct for all staff and other adults in the program (45 CFR §1302.90). The use of restraints or isolation to discipline a child are strictly prohibited. As the disabilities lead, you need to know these regulations to ensure your program takes the appropriate actions.
Depending on the situation, you and the team may decide to engage community mental health resources.
Children who receive IDEA services have additional protections from suspension and expulsion under the law. IDEA states that programs serving 3- to 5-year-olds must make reasonable modifications to policies, practices, or procedures to protect children with disabilities from suspension or expulsion for disability-related behaviors, unless a program can demonstrate that making such modifications would fundamentally alter the nature of a service, program, or activity. If the child's behavior impedes the child's learning or that of others, the IEP team must consider behavioral intervention strategies and supports. For example, the Pyramid Model is often used in Head Start programs.
As your program considers alternatives to suspension and expulsion, it's important to ask the following questions:
- Are these options in the best interest of the child and family?
- Do they ensure the child's full and effective participation in the program?
If the answers are "no" because they don't maximize the child's learning opportunities, these are not viable alternatives. This often means that a child can't be moved from a center-based program that offers interactions with peers to a home-based program. The needs of the family must be considered, too. If they need the support of a full-day program, a home-based program is not an acceptable alternative. If the child has an IEP, the decisions must support the child's IEP-mandated services in the LRE. As the disability services coordinator, you are a strong advocate for inclusion of children with mental health concerns.
The key pieces of legislation—IDEA, Section 504 of the Rehabilitation Act, and ADA—prohibit discrimination and exclusion on the basis of a disability.
Turn to program management; the mental health consultant; and health, education, and family service staff. Together, consider ways to provide individualized support to the child and family.
- Conduct a functional assessment to provide more systematic data to make decisions.
- Make sure the routines and curriculum activities are developmentally appropriate.
- Ask the family about the child's behavior at home and find out what works for them.
- Use coaching, mental health consultation, or other professional development activities to build staff competencies and confidence.
- Consider referring the child to the local IDEA agency responsible for determining whether a child can receive services. A formal evaluation may provide a mental health diagnosis and specify intensive support in an IFSP, IEP, or Section 504 Plan.
- Develop an internal Child Action Plan while waiting for the evaluation results. If the child does not receive services, continue with the plan.
- Consult with the IDEA agency if the child already has an IFSP or an IEP to ensure the child is receiving the support services specified.
Document the steps you've taken to include the child in the Head Start program. The family, teachers, IDEA agency, and mental health consultant can use the information to determine whether the child needs a more appropriate placement. Your program must collaborate with the parents and professionals to transition the child.
A useful resource for educational staff is the Pyramid Model. It's a tiered framework of evidence-based interventions that promote children's social, emotional, and behavioral development.
Tips to Promote Quality Health and Mental Health Services for Children with Disabilities
Many of these tasks are coordinated with the health manager and health staff.
- Review screening results for health and mental health concerns. Discuss with the managers whether a child needs a referral for an evaluation with the local IDEA agency or with a medical or mental health provider.
- Review daily health and attendance records. Note changes in health status and increased absenteeism of children with disabilities and special healthcare concerns. Talk to families, education staff, and special education partners to make any accommodations necessary to ensure a child's full and effective participation.
- Promote oral health. Work with the health manager to help staff learn how disabilities can affect oral health and develop routines and strategies to ensure children with disabilities brush their teeth. Make sure children get necessary follow-up treatment.
- Promote nutritional health. Work with the health manager and nutritionist to review menus and identify accommodations for children with disabilities during mealtimes. Assist families to access food appropriate to their child's dietary needs.
- Partner with the mental health consultant. Work together to identify program needs and effective consultation supports.
- Review HSPPS regulations about suspension and expulsion. Ensure staff understand the program's policies and how they apply to children with disabilities or suspected delays. Commit to keeping children enrolled in your program.
- Ensure individualized teaching and learning. Help staff respond effectively to children whose behaviors are challenging to adults. Include all personnel who come into contact with the child, including transportation, nutrition, and health staff.
- Support staff to implement medical procedures. Work with the health manager to ensure staff understand necessary procedures related to special equipment, wheelchairs, or modifications to routines. Develop a protocol for staff to contact you or the health manager for help.
- Check on effective service delivery for children with IFSPs and IEPs. Ensure the specified services are being delivered to children who have health or mental health disabilities.
- Respect cultural beliefs and values about health and mental health. Ask families about their health practices and their views about mental health. Help them address stigmas or stereotypes they or other family members may have.
- Advocate for the representation of medical and mental health services on the HSAC. Ensure the committee includes specialists who are knowledgeable about disabilities and who can speak on behalf of families.
- Use community resources. Invite health providers to inform staff about health and mental health concerns in early childhood and effective strategies.
 People to Help You
People to Help You
- Health manager and staff
- Program leaders and managers
- Family services manager and family advocates
- Education managers, teachers, and home visitors
- Nutrition staff
- Mental health consultant
- HSAC
- T/TA providers
- Community partners
- Families
Questions to Ask Your Colleagues
- How do we include children with disabilities in our health services planning?
- How do we access health information for children with disabilities?
- How do we work with medical and dental providers of children with disabilities?
- How do we screen children with disabilities for health concerns?
- Are we satisfied with our screening procedures for social, emotional, and behavioral concerns?
- How do we use our ongoing assessment data to identify mental health concerns?
- What do our staff and families need to know about the relationship between disabilities and social and emotional development?
- What is our social and emotional curriculum?
- What are our discipline policies?
- How do we prevent the suspension and expulsion of children with mental health concerns?
- Do we implement highly individualized practices to support children whose behaviors challenge us? What more do we need to learn about effective strategies?
- How do we work with the mental health consultant? What kinds of support do we need from the consultant?
- What supports do our staff and families need to promote their own physical and mental well-being?
- What is the best way to access the HSAC? Who serves the child and why?
- Which community partners provide medical and mental health supports? How are families referred?
- How can we improve our collaborations and partnerships?
Scenario
Four-year-old Tony has a feeding tube. His IEP specifies nutrition support and inclusion with his peers during mealtimes. His parents provide valuable information about their techniques at home. The health manager develops protocols to use with Tony. All of this is a new experience for the teacher, Nury. She asks to meet with the disability services coordinator, the health manager, and her education supervisor. Nury wants their help to ensure mealtime is a positive learning experience for Tony and that other children engage with him. She knows she needs to build her confidence.
First, the support team suggests that Nury observe at lunchtime to see how to embed learning opportunities for all the children. In fact, she finds that lunchtime offers many opportunities to address the children's questions about Tony's device. Also, this is a time to reinforce curriculum goals, such as building empathy and understanding and communicating.
The support team also suggests ways to embed learning opportunities in the classroom curriculum. Working with Nury, they obtain materials similar to Tony's feeding tube for the dramatic play area. In the context of peer play, the children can learn about Tony's experiences. The team considers other centers in the classroom, including the language and literacy area. Nury asks the school librarian to help her find books about young children with health problems and their coping strategies. When Tony goes to the hospital for a few days, the class illustrates a "Welcome Back" book for him when he returns to class. He is thrilled, and so are they!
1 In this guide, the term children with disabilities includes children with suspected delays, unless stated otherwise.
2 Section 504 of the Rehabilitation Act covers some children with disabilities.
Read more:
Resource Type: Article
National Centers: Early Childhood Development, Teaching and Learning
Last Updated: July 13, 2021